What steps should employers (and everyone else) be taking now to prevent the spread of COVID-19? Read on for quick facts, tips and best practices to help you and your team members reduce the risk of infection at work and at home.
What you will learn:
- Quick Facts - Introduction to COVID-19
- Quick Facts - Common and severe symptoms
- Quick Facts - How it spreads and who is at risk
- Quick Facts - How testing works and testing locations
- Quick Facts - Instructions for D.C. Metro Area
- Employers - Best practices for the workplace
- Employers - Emergency response planning
- Employers - Business interruption insurance
- Individuals - Understand how the virus spreads
- Individuals - Disinfecting surfaces
- Individuals - Follow sanitation guidelines
- Individuals - What to do if you experience symptoms
COVID-19 Overview.
What is Coronavirus/COVID-19?
According to the Centers for Disease Control (CDC), Coronavirus refers to a large family or group of viruses that affect humans and other mammals, including bats, cats, cattle, and camels. Sometimes, a coronavirus can spread between people and other animals. Other "famous" coronavirus outbreaks include MERS-CoV, which causes Middle East Respiratory Syndrome/MERS, and SARS-CoV, which causes Severe Acute Respiratory Syndrome/SARS.
The current outbreak involves a novel (or new) coronavirus, identified by the CDC as COVID-19.
On March 11, the World Health Organization (WHO) declared COVID-19 a pandemic. According to National Public Radio, this is the first such WHO declaration since the H1N1 or "swine flu" of 2009.
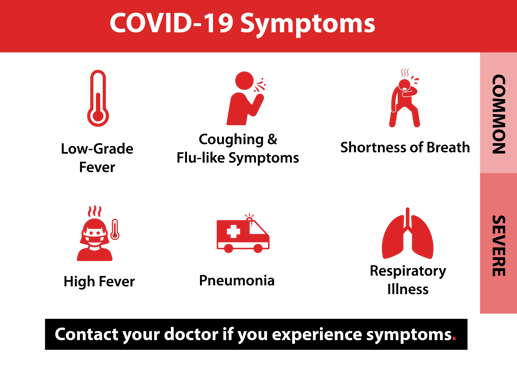
What are the Symptoms of COVID-19?
Symptoms appear from two to 14 days after exposure to the virus. According to the CDC, the most common COVID-19 symptoms include: fever, coughing, and shortness of breath. More severe cases may experience lung infections (pneumonia) and other respiratory issues.
How Does COVID-19 Spread?
Experts believe that the virus spreads through person-to-person contact. This means it may spread when people are within close proximity (about 6 feet) to an infected person. The virus may spread when a sick person emits droplets by breathing, coughing or sneezing, then the droplets enter someone else's nose, mouth or eyes.
The virus can also spread if someone touches a contaminated surface, then touches their face.
The incubation period for the novel coronavirus is estimated between 2 to 14 days after exposure. According to a recent report by the Annals of Internal Medicine, more than 97% of people who contract the virus show symptoms within 11.5 days of exposure.
Who is Considered High-Risk?
While anyone can contract COVID-19, most patients experience mild symptoms. Those most at risk of developing severe symptoms or complications are:
- Older adults
- Those with chronic health conditions such as heart disease or diabetes
- People with respiratory illnesses
- Those with compromised immune systems
- People engaging in domestic or international travel
Individuals in these groups should take extra precautions to reduce the likelihood exposure.
COVID-19 Testing: How it Works and Where to Get Tested
The test for COVID-19 is conducted much like a standard flu test. These tests look for certain types of RNA that indicate the presence of the virus, according to Stanford University Medicine. The testing process involves swabbing the patient's nasal cavity to collect cells.
NBC News has contacted all 50 state health departments for more insight into how each state is handling testing and the guidance they are offering individuals who seek tests.
G
eneral advice is consistent nationwide: Call your doctor or healthcare facility if you are concerned you may need to be tested. Based on your symptoms and exposure, they will decide if you need to be evaluated in person and may confer with state authorities about where and how to do the testing.
Furthermore, NBC News is relaying specific testing instructions for each state. Below are instructions for the Washington D.C. metropolitan region. If you live outside this region, see their article for testing information pertaining to your state.
In addition, the Association of Public Heal Laboratories (APHL) has published a list of testing locations throughout the country with the following instructions for the D.C. Metro Area.
DISTRICT OF COLUMBIA:
- Call your primary care doctor or a healthcare facility if you are experiencing respiratory symptoms to be evaluated for testing. Residents without a primary care provider can call 202-576-1117. Call ahead before arriving at any medical facility in person.
- If you think you have symptoms, stay home from work or school until you are free of fever, signs of a fever and any other symptoms for at least 24 hours and without the use of fever-reducing or other symptom-altering medications.
- Patients who meet the CDC's criteria based on exposure and clinical factors and who are pre-approved by DC Health will be tested through the DC Department of Forensic Sciences Public Health Laboratory.
- For more information, visit DC's coronavirus website and resource page.
MARYLAND:
- Call your healthcare provider if you are symptomatic to discuss whether you should be evaluated in person and considered for testing. Call ahead before going to any healthcare facility.
- Testing is appropriate for those who are at highest risk for developing severe COVID-19 disease. People who are mildly ill should not go to emergency rooms but stay at home and call their health care provider for guidance.
- Your provider will decide if you should be tested based on several factors, including their clinical judgment, and the availability of testing supplies and lab resources.
- When they deem appropriate, providers order tests and collect samples, which they then send to a laboratory for testing.
- There are multiple labs conducting testing in the state. Results time varies depending on the lab.
- For more information, visit the Maryland Department of Health's coronavirus website.
- Call your healthcare provider if you are symptomatic to discuss whether you should be evaluated in person and considered for testing. Do not go to your local health department for testing.
- Your provider will work with your state or local public health department and the CDC to determine if you need to be tested.
- To be tested at the state public health laboratory, patients must meet the state's criteria, which evaluates a combination of symptoms and risk factors. Alternatively, patients can consider testing at commercial labs, which don't have set requirements and don't need an approval from the state’s health department.
- Results from the state's public health lab are generally available within 24 hours.
- For more coronavirus information, visit the Virginia Department of Health's website.
What Can Employers Do?
It is crucial for employers to implement precautions in the workplace to prevent the spread of the virus. In addition, all organizations should prepare a response plan.
Implement these Best Practices
- Offer Non-Punitive Sick Policies. As medical facilities are overburdened, consider not requiring a doctor’s note.
- Practice Social Distancing. As the virus is contagious even before symptoms show, a person can spread the virus to others without knowing. Therefore, encourage employees to limit their exposure to others whenever they can. Telework is strongly recommended to reduce pathogen transfer.
- Intensify Cleaning Routines. Focus on surfaces that are frequently touched (keyboards, door handles, countertops, etc.) and consider making cleaning supplies easily accessible to everyone.
- Encourage Smart Hygiene. Employees working in the office should wash their hands with warm water and soap for at least 20 seconds and avoid touching their face.
- Create Sanitation Bubbles. Provide hand sanitizer stations for employees when they enter and exit the office and encourage them use hand sanitizers in their homes and cars.
- Review Travel Guidelines. Check the CDC’s Traveler Health Notices for country and region-specific information.
- Maintain Open Communication. Clear communication between management and staff during this critical time is critical to limiting business interruption and limiting errors.
Create a COVID-19 Response Plan
A clear response plan will help your business implement prevention strategies while ensuring business continuity.
You must be prepared for staff to work remotely and your operations must be able to continue with limited staff. Your response plan should:
- Identify possible health risks
- Outline prevention strategies
- Establish communication protocols
- Describe what you'll do if an employees contracts COVID-19
- Ensure human resource policies are inline with government regulations
- Engage state and local heal departments
Business Interruption Insurance Coverage
Many businesses are feeling either direct or indirect financial consequences of the COVID-19 pandemic. They are subsequently asking if their Business Interruption Insurance policy will be providing coverage for lost income due to the disruption. Unfortunately, the policy is not designed to provide coverage in the event of a pandemic.
Also referred to as "loss of income" insurance, this policy requires physical damage to take place for a business to file a claim for loss of income, which is not the case with the COVID-19 outbreak.
However, in the event that there is a government-mandated shutdown of your business, there could be financial relief for business interruption provided by the federal government.
Stay tuned for updates on business interruption coverage.
What Can Individuals Do to Stay Healthy?
Understand How it Spreads
A recurring theme among the experts is that avoiding exposure is simply the best way to prevent illness. Understanding how to avoid exposure is therefore the first precaution individuals can take.
For example, stay mindful that the virus is currently thought to spread from person-to-person - especially within 6 feet of proximity or less. One may also contract the illness through respiratory droplets when someone infected coughs or sneezes.
The next time you are outside or inside, remember to guard yourself against potential exposure when someone near you coughs or sneezes.
Although you may see people wearing face masks, the CDC only recommends you wear one if you're already sick. Most face masks don't prevent you from getting the virus, though they may slow the mask wearer from spreading the virus to others.
Remember to Disinfect Surfaces
Avoiding surfaces is another crucial precaution. NPR cited this recent study conducted by the Cold Spring Harbor Lab that reports the virus can survive on surfaces on plastic and stainless steel for up to 72 hours and on cardboard for up to 24 hours.
At home and work, disinfect frequently touched surfaces. Focus on door handles, counters, laptops, screens, phones, and other work surfaces that get a lot of use. Use a disinfecting household cleaner and follow the label instructions.
Practice Social Distancing
If you're at a higher risk of infection, do your best to practice "social distancing." That means avoiding public and crowded spaces, staying home when possible, and avoiding exposure.
Be Vigilant with Hygiene Routines
Staying clean and consistent with your disinfecting routines will also help you keep those around you safe. Consider the following self-disinfecting suggestions:
- Wash your hands with warm soap and water for at least 20 seconds after using the restroom, touching surfaces, coughing, sneezing, blowing your nose, before and after preparing food
- If soap and water are not available, use disinfectants containing least 60% alcohol
- Avoid close contact with others and try to maintain personal space of at least 6-10 feet
- Avoid touching your face, as the virus can spread from your hands to your mouth, nose and eyes
- According to Time, cellphones are 10 times dirtier than toilet seats. Keep your phone out of restrooms and disinfect it on a regular basis.
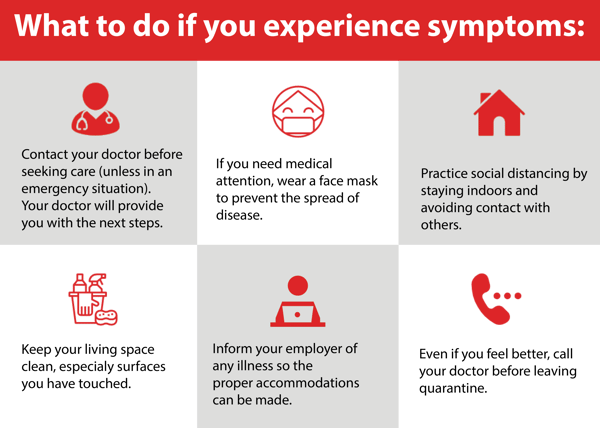
What Should You Do if You Get Sick?
If you're feeling ill, the CDC recommends calling your doctor before seeking care. (Of course, if you're having trouble breathing or are very ill, seek medical care immediately.) Your doctor can tell you what your next steps should be and alert the local health department if necessary. If you do go a medical facility, that's a good time to protect others by wearing a mask.
Once you've sought medical care, stay home. Avoid people and animals, and don't share household items (like plates, utensils and bedding) with others. Keep your surroundings clean, especially surfaces that you've touched.
It is critical that you let your employer know if you experience any developments with your health, be it the common cold or a positive test for COVID-19. This will allow your employer to implement proper precautions and procedures as soon possible to limit any new infections among staff.
Given how quickly COVID-19 spreads, employers should take a proactive approach to protect their staff, business, communities, and their own health. Washing hands, keeping workspaces clean, developing a response plan, and keeping the lines of communication open are key to prevention.
As the virus can be deadly for the elderly and those with health problems. Taking preventive steps now will help "flatten the curve" and slow the rate of transmission. In the end, that benefits everyone.

.png?width=2000&name=LET%20US%20HELP%20(2).png)


